Avoid camping/backpacking/hiking if you are feeling ill or if your animal companion is ill. People and animals are more prone to disease if their immune systems are weakened by other illnesses or conditions.
Keep your outdoor gear (including tents, netting, sleeping bags, etc.) in good condition and repair or replace damaged items.
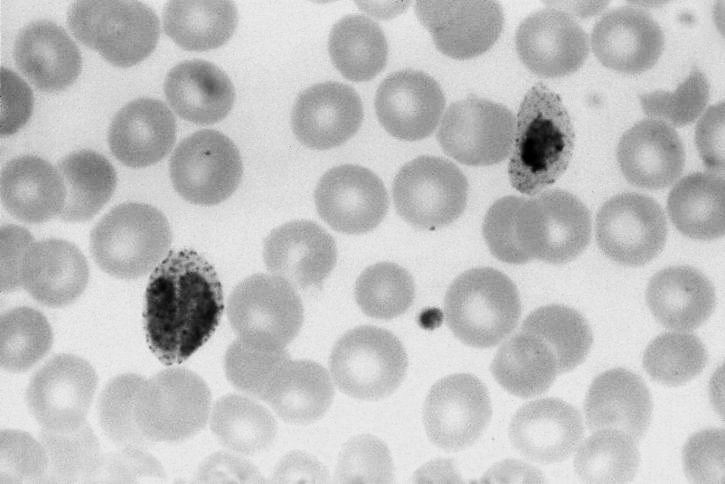
Take precautions to minimize insect bites.
Wash hands thoroughly with soap and water or an alcohol-based sanitizer immediately after handling animals, soil, equipment, or food.
Wash tools, cooking equipment and working surfaces (including tables and cutting boards) thoroughly with soap and water after use. If contamination with soil or animal feces (stool) is suspected or known, disinfect the equipment and surfaces immediately. Adding a minimum of 1 tablespoon of bleach to 1 gallon of water is usually adequate for use as a cleaning/disinfecting solution.
Avoid eating raw or undercooked meat.
In the United States, campers and hikers/backpackers should report any signs of sick wildlife or wild bird die-off to the state's game and fish agency or wildlife agency.
Make sure your animal companions are up-to-date on their vaccines, especially rabies, prior to camping/hiking season.
Consult your veterinarian about proper preventive treatments for your animals, such as heartworm prevention for dogs and cats, and use the products as recommended.
Consult your veterinarian about regular stool exams of dogs to check them for parasites, including those that can be passed to people.
Do not allow your dog to eat dead wildlife.
Outdoor enthusiasts who regularly travel with animal companions should consider getting some basic training in human and animal first aid techniques. In addition, carrying a first aid kit with supplies for humans and animals is extremely important.
To protect your dogs, you should consult your veterinarian, but basic guidelines include:
Apply topical or systemic tick-control treatments. Consult your veterinarian about the appropriate product for your dog.
If possible, limit access to tick-infested areas.
Check dogs frequently for ticks or, at a minimum, at the end of each day's activities. The ticks should be promptly and carefully removed.
To protect your horses, you should consult your veterinarian, but basic guidelines include:
Apply topical insect repellent products. It is likely you will have to reapply the products regularly, especially if you are traveling through areas with high insect activity.
If possible, limit access to tick-infested areas.
Check horses frequently for ticks or, at a minimum, at the end of each day's activities. The ticks should be promptly and carefully removed. Be sure to check the tail, mane and ears thoroughly for ticks.
Consider the use of insect nets designed to be worn over horses' eyes and ears to minimize insect bites, but do not consider them 100% effective. If you use these products, you should still check your horses regularly for ticks.
Hear From Us Again
Don't forget to subscribe to our email newsletter for more recipes, articles, and clinic updates delivered to your inbox (here). Or, you can keep up to date by liking and following our Facebook page (here).
Related: We have more information under our dog health + cat health categories.