Disease of the Optic Nerve in Dogs
Glaucoma is a condition in which pressure is placed on the eye, causing inadequate fluid drainage in the eye. If the condition becomes chronic or persists without treatment, it will eventually cause permanent damage to the optic nerve, resulting in blindness.
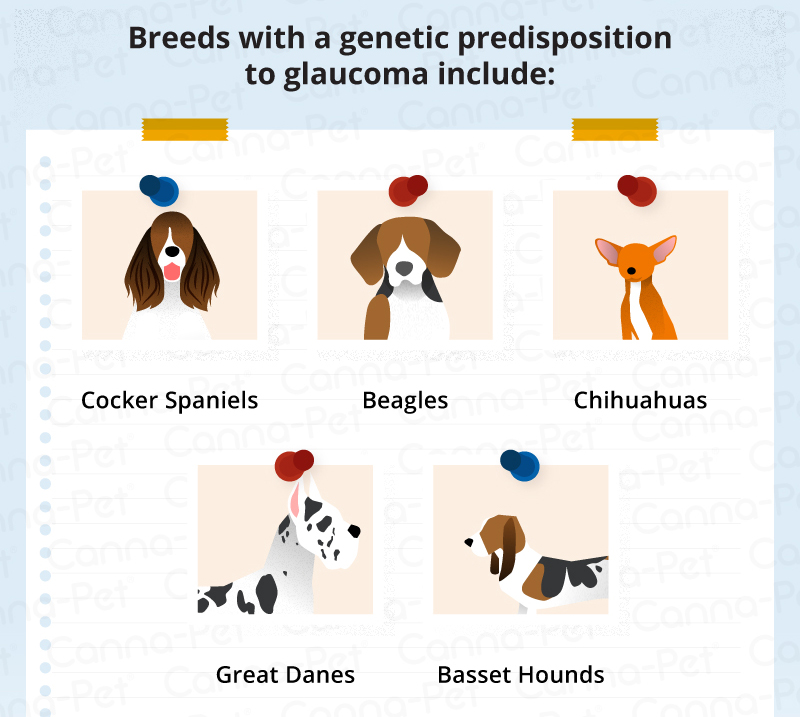
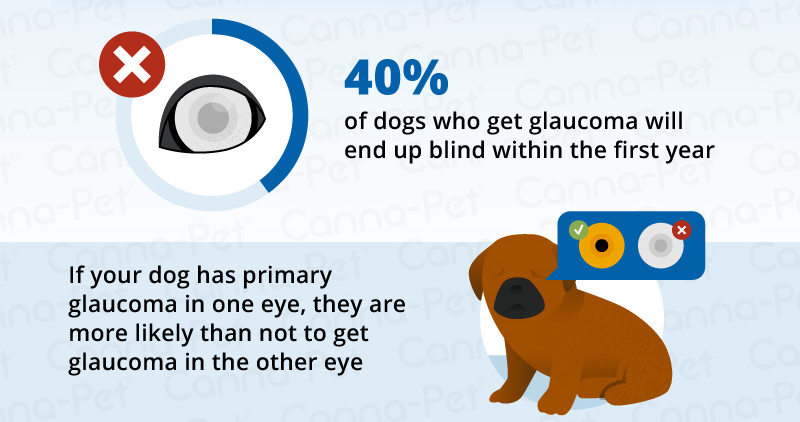
Glaucoma is common in certain dog breeds that are genetically predisposed, such as samoyeds, cocker Spaniels, poodles, chow chows, and Siberians. Unfortunately, 40% of dogs affected by glaucoma will become blind in the affected eye within the first year, regardless of medical or surgical treatment.
Symptoms and Types of Glaucoma
There are two main types of glaucoma: primary and secondary. Symptoms for sudden primary disease, due to the eye's inability to drain through the filtration angles of the eye, are as follows:
High pressure within the eye
Blinking of the eye
The eyeball may recede back into the head
Redness of the blood vessels in the whites of eyes
Cloudy appearance at front of the eye
Dilated pupil – or pupil does not respond to light
Vision loss
Long-term, advanced disease:
Enlargement of the eyeball (buphthalmos)
Obvious loss of vision
Advanced degeneration within the eye
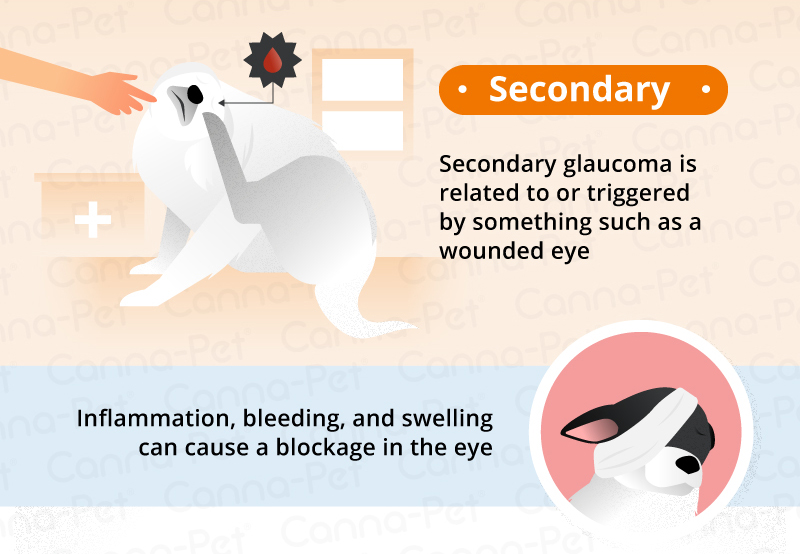
Symptoms for secondary glaucoma, or glaucoma due to secondary eye infection(s), include:
High pressure within the eye
Redness of the blood vessels in the whites of eyes
Cloudy appearance at front of the eye
Inflammatory debris visible in the front of the eye
Possible constriction of the pupil
Possible sticking of the iris to either the cornea or the lens
Possible that the edge of the iris circularly sticks to the lens
In addition, there may be:
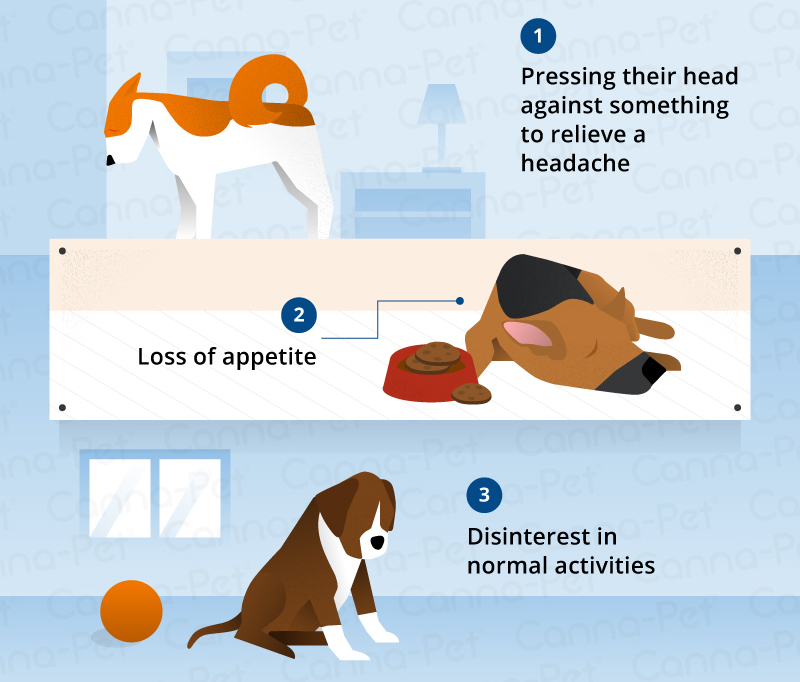
Headaches, with head pressing to relieve feelings of pressure in head
Loss of appetite
Change in attitude, less desire to play or interact
Causes
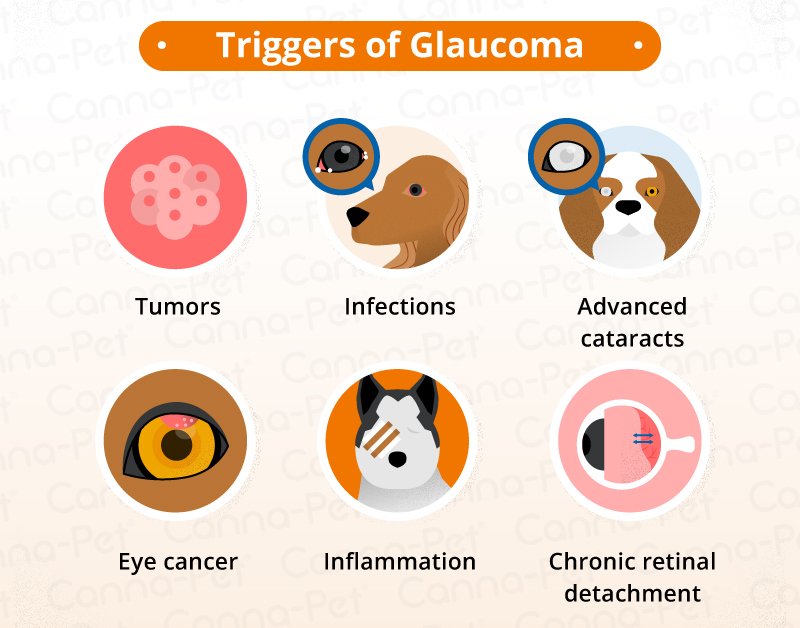
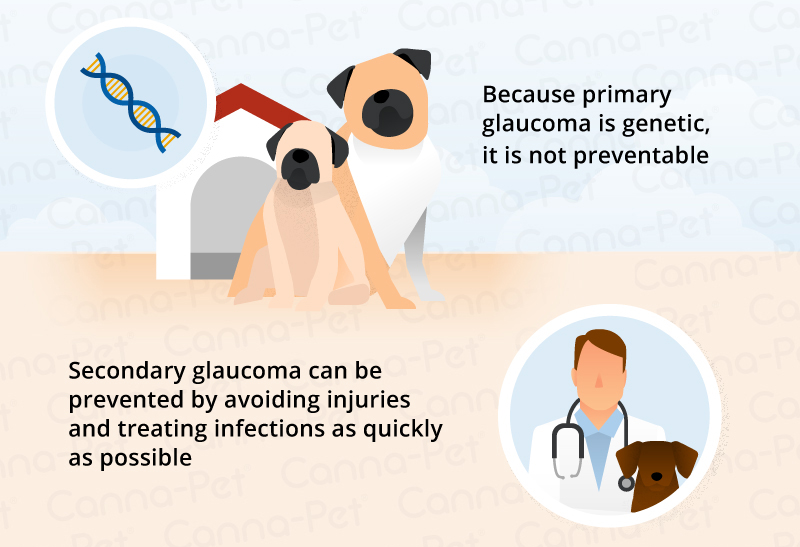
High pressure in the eye occurs when the normal outflow of fluid in the eye is impaired due to a primary eye disease such as the improper development of the eye's filtration angles, or secondary to other eye diseases such as primary lens luxation (slipping of the lens in the eye), inflammation of the tissues of the eye, eye tumor(s), or blood collection in the front of the eye from injury. In dogs, secondary glaucoma is more common than primary glaucoma.
Diagnosis
You will need to give a thorough history of your dog's health, onset of symptoms, as far as you have been able to tell, and possible incidents that might have preceded this condition, such as injuries to the eye (even those which you consider minor). During the physical examination, your veterinarian will test the pressure within your dog's eyes using a tonometer on the surface of the eye. If the disease began suddenly, your veterinarian will refer your dog to a veterinary ophthalmologist for a detailed examination of both eyes, including evaluation of the filtration angles by gonioscopy -- measuring the anterior of the eye. Pressure within the eye can measure as high as 45 to 65 mmHg, making this a very painful condition.
Electroretinography will be also performed by the veterinary ophthalmologist to determine if the eye will remain blind despite treatment. In secondary diseases, X-rays and an ultrasound may show abnormalities within the eye.
Often both eyes are affected, but not always. In cases where only one eye is affected, steps will be taken to protect the unaffected eye from developing a diseased condition.
Treatment
It is helpful to think of treating glaucoma like a major medical emergency. The faster and earlier you address the problem, the least likely your pet is to suffer maximum, sustained damages. The top three goals are to reduce pain, drain excess fluid, and reduce how much aqueous humor the eye produces.
Most treatments are geared toward pain management to help ward off the headaches associated with glaucoma, and in delaying or preventing the disease from happening in the second eye. Your vet may recommend performing a gonioscopy to determine your best shot at saving the remaining eye.
Reduce aqueous humor fluid.
Some treatment options seek to decrease the amount of fluid the eye produces, since draining the eye and keeping it drained can be tough, if not impossible in animals. There are pills and eye drops used for these purposes, and although they are helpful, they aren’t that great as a long-term option, and are ineffective in an emergency. The medications are most useful as a Band-Aid method until surgery of the affected eye is possible. This combination of treatment methods is usually the pet owner’s best chance at saving their dog’s vision.
Reduce stress.
As with humans, stress can be very detrimental to a dog’s health. The immune system cannot do its job and the body cannot fight off oxidative damage if stress levels are high.
Avoid treating a blind eye.
Medical treatment of an eye that’s already blind is not recommended. There’s no point in paying for expensive drugs and therapies to try to recover sight that is impossible to recover. In some cases, it might just be best to remove the blind eye entirely in order to mitigate pain and discomfort. It’s cheaper than the cost of medications and ongoing visits with the vet for eye exams.
Hear From Us Again
Don't forget to subscribe to our email newsletter for more recipes, articles, and clinic updates delivered to your inbox (here). Or, you can keep up to date by liking and following our Facebook page (here).
Related: We have more information under our dog health tags.